Lingual, labial frenums: Early detection can prevent health effects associated with tongue-tie
Early detection can prevent cascading health effects associated with tongue-tie
By Martha Macaluso, MLT, RDH, BS, and Dana Hockenbury, CCC-SLP, COM
Ankyloglossia, also known as tongue-tie or TOTs, is a congenital oral anomaly that may inhibit the mobility and proper function of the tongue. This is caused by an unusually thick, tight, or short lingual frenulum, a membrane that connects the underside of the tongue to the floor of the mouth.1 There are many variations and differing degrees of severity.4,6,7,11 Prevalence of tongue-tie in the United States is 3% to 4% among newborns.1 Studies cite a male preponderance with ratios varying from 1.5:1 to 2.6:1.1,7
• The maxillary midline frenum
• The mandibular midline frenum
• The right and left upper and lower labial frenums
• The lower lingual frenum
The primary function of frenums is to keep the lips and tongue in harmony with the growing bones of the mouth during development.7 The frenums of most concern are those found under the tongue, front upper lip, and front lower lip.
These anomalies are historically overlooked in the hospital and clinical settings, causing detrimental effects in an infant's ability to latch on to their mothers during breastfeeding. Often clicking sounds during feeding can be heard caused by the tongue's recoil.4 This indicates that the baby is repeatedly breaking the seal or suction during feeding. This inability to latch onto the breast has many consequences on an infant, such as inability to thrive, malnutrition, and colic among other cascading health effects such as orofacial myofunctional disorders (OMDs). If left undiagnosed, these consequences can lead to further physical and developmental problems which will carry on throughout adulthood.
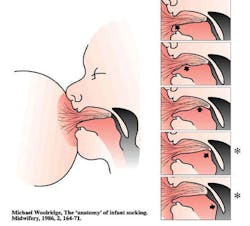
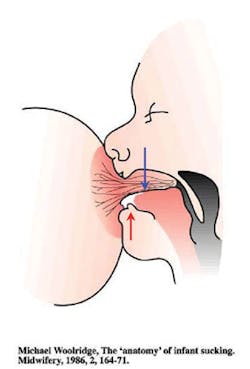
Normal tongue position during breastfeeding.Infant with lingual frenum restriction during breastfeeding.
Importance of Normal Breastfeeding
Proper breastfeeding benefits have been attributed to the promotion of adequate oral motor development, which has a positive effect on growth and craniofacial development. During feeding, intense movement of the lips, tongue, upper and lower jaws, and cheeks occurs with positive effects on the infant's oral motor development. The jaw movements involved in extraction of milk from the breast provide stimulation for growth of the temporomandibular joint and, consequently, encourages forward growth and development of the facial region, most importantly the maxilla and mandible.
The muscles involved in breastfeeding, particularly the masseters, are the same muscles that will later (from the age of six months onward) carry out chewing and swallowing. Therefore, chewing continues the process of stimulation of the orofacial muscles that begin with sucking at the breast. Correct sucking, chewing, and swallowing plays a role in the development of the upper and lower jaws. Together with genetic and environmental factors, this provides stability of the dental occlusion, function, and muscle balance.9
The tongue is one of the most critical organs in our bodies. The tongue has the ability to shape our palate, influences the way our teeth are seated in our mouth, regulates our posture, drives our speech, determines the opening of our airway, and develops our facial structure. Its base, which is located in the throat, has the ability to shape our throat muscles. The rest of the tongue, which is located in the center of the oral cavity, is critical and essential in developing the upper jaw, the shape of our face, and our upper airway nasal passages. Thus the position of the tongue in the oral cavity is critical to proper dentofacial growth and development.
Tongue Restrictions
When a tongue restriction or tongue-tie is present, the tongue tip, blade, and/or sides of the tongue can't reach vertically to make contact with the hard palate to create a light suction.7 This inability of the tongue to reach the roof of the mouth during rest or swallowing will contribute to an abnormal tongue-resting posture (low and forward), and an abnormal swallowing pattern (tongue thrust) among other health and dental effects in the future. The entire body will then begin to accommodate to this incorrect tongue-resting posture, contributing to facial esthetic changes, forward head posture, and mouth breathing to name a few. It is well documented that the tongue-resting posture plays the most critical role in facial developmental changes because it is the most constant.
The presence of an abnormal tongue posture sets the stage for orofacial myofunctional disorders (OMDs), and later airway problems such as obstructive sleep apnea (OSA).
Selectively chosen from the "Lingual Frenulum Protocol With Scores For Infants" to demonstrate varying degrees of lingual frenulum thickness and attachment.
OMDs are muscular disorders that directly and indirectly affect the development of the face, jaws, and teeth along with a variety of functions, such as chewing, swallowing, speech, oral hygiene, occlusion, temporomandibular joint movement, stability of orthodontic treatment, facial esthetics, and facial skeletal growth.16 Facial skeletal growth is nearly complete (90%) by the age of 12, with some minor changes occurring thereafter.15 Changes in throat tone, palatal shape, and craniofacial misalignment generate poor tongue posture and mouth breathing; which in turn contribute to weakness of the throat musculature. Over time, muscular weakness can cause airway collapse and the formation of obstructive sleep apnea.15
As stated in the literature, speech problems may also develop from restricted lingual frenums. Individuals develop a very poor sense of the geography of the mouth, because they have such a limited range of lingual movements. They can be difficult to correct by conventional means because they cannot memorize the correct movements of speech, or be sure of always achieving them. Adults develop methods of speech which mask their difficulties with sound production.8
Both adults and children often try to speak with a small opening, so that they can make the lingual contacts required for pronouncing specific consonants; others speak slowly, softly, or loudly. Nearly all people with restricted frenums past toddler stage are aware of the movements their tongue cannot make. Clarity in rapid speech is almost always impossible for a tongue-tied person to achieve.8
The restrictions that a tongue-tie causes may vary from patient to patient, but movements-such as lingual elevation to the upper teeth and horizontal lingual protrusion-are consistently difficult or impossible to achieve because of the pull of the tight lingual frenum on the floor of the mouth and on the tongue.8
This inability to move the tongue or the lips in an appropriate manner while speaking can affect a variety of sounds:
• The T, D, L, N, R, TH sounds in English
• The Z, SH, R, TS, D, T, L, N sounds in Hebrew
• The D, L, R sounds in Finnish
• The rolling R in Spanish8
In addition to poor speech sound development, drooling while speaking may also be observed. Incorrect articulatory compensatory habits may develop which may cause other detrimental effects later in life. This universal inability to communicate properly may potentially lead to behavioral problems in a child as well.8
Lip Ties and Their Impact
When the maxillary frenum of the upper lip is restricted, it can also cause multiple problems and concerns. As with tongue-ties, there are various levels of restriction with maxillary (upper) lip ties.3 These upper lip ties can negatively impact upon the infant's ability to latch on to the breast while feeding. The upper lip needs to flange upward with a wide mouth to create a seal while sucking. Typically, the lips should extend 1 to 1.5 inches beyond the nipple.4
Without adequate lip seal, air is taken in during the suck/swallow/breathe sequence, resulting in gastric reflux, abdominal distension, belching, flatulence, and fussiness. Colic symptoms can be observed. Often, the infant is prescribed medication to address the reflux. This is an unnecessary burden since, once the restriction is eliminated, the reflux is reduced or disappears, eliminating the need for medicine.4
Without an adequate lip seal, slipping off the breast, nipple pain and trauma, blocked ducts, nipple and breast infections,5 short, frequent, and unproductive feedings, and ultimately failure to thrive2 will result. Prematurely switching to bottle feeding ensues.
As the child grows and the maxillary lip tie is not released, habitual mouth breathing may develop, contributing to other unrelated ailments such as an abnormal swallowing pattern, low tongue-resting posture, dental caries, periodontal disease, gingival recession, malocclusions, and diastemas to mention a few.3,7
Assessment - "Because a tongue-tie has been defined as an anatomical anomaly that adversely impacts tongue function, assessment ought to include evaluation of tongue function as a primary goal."15 Unfortunately, when just performing a visual cursory exam, some ties will be missed, contributing to the previously outlined detrimental effects as the infant develops.
A comprehensive clinical examination of the restriction and function must be made in order to determine the severity of the tongue and/or lip restriction. Only then will the recommendation for appropriate surgical intervention be made followed by proper wound care.
Various comprehensive diagnostic tools have been developed for proper assessment of lingual and labial frenums, and should be incorporated as part of an accurate assessment such as:
• The "Lingual Frenulum Protocol with Scores for Infants," developed by Martinelli for tongue and lip screening
• "The Lingual Frenulum Protocol" by Marchesan
These protocols are used widely in Brazil, which is the first country in the world to mandate frenum inspections as part of the infant screening protocol. Unfortunately, frenum inspections as part of the infant screening protocols are still lacking in the United States and other countries.
Postoperative wound care - The mother is instructed to conduct postop stretching exercises three times a day for three seconds for six days postop.6 It is highly recommended that the mom practice with her baby one week prior to the procedure so mom and infant can get used to the movement and the action.5
Place the infant's head on the examiner's lap, facing toward the parent as the parent gently holds the arms. Place fingertips under the tongue and press downward toward the throat to see the area open and view the entire diamond shape of the area. A second method recommended by the author that may be easier for many parents is to place a tongue blade at the base of the tongue. Using the tongue blade, push up on the tongue. Simultaneously, with the other hand, push down on the lower jaw with adequate pressure to open up the diamond shape wound. This should be done twice a day, usually prior to morning feeds and evening feeds either just prior to breastfeeding or when the infant is being switched from one breast to the other. It is also recommended that, prior to each feeding, the mother sweep the tip of her finger across the floor of the mouth, opening the area.
In addition to completing daily stretching of the tongue, facial and lip massaging is recommended by Kotlow to help reduce stressed and tight facial and lip muscles. The author recommends that the mother gently massage the cheeks for the first week after surgery. A second massage to facilitate a proper suck and latch is to use a finger in a circular motion around the lip, slowly allowing the infant to root for the finger.
Kotlow also recommends conducting stretching exercises postop to prevent scarring at the wound site.7 For the adult patient, Babu14 recommends a variety of stretching exercises similar to those recommended for children. The following exercises were advised:
• Stretch the tongue upward toward the nose, then down to the chin, and repeat
• Open the mouth widely and touch the big teeth with the tongue and the mouth open
• Shut the mouth and poke the tongue into the left and right cheek to make a lump
These exercises should be conducted for three- to five-minute bursts once or twice daily for three to four weeks postoperatively.
Early intervention to correct aberrant lingual and/or labial frenums is essential in order to attain proper oral balance. A multidisciplinary approach must be taken in order to help prevent cascading detrimental health effects. A team of qualified professionals such as dental hygienists, speech pathologists, dentists, myofunctional therapists, lactation consultants, and medical doctors can aid in preventive care and early diagnosis.
The dental hygienist possesses a critical role when a patient is in the dental chair. Being able to examine and identify these restrictions can help prevent lifelong detrimental effects caused by these restrictions.
All newborns should be examined and the need for frenectomy identified as soon as possible after birth. Early intervention to correct aberrant lingual and labial frenums will improve breastfeeding and avoid later problems with tooth, jaw, and speech development. Early diagnosis and release of the lingual, mandibular, and maxillary lip frenums can prevent these issues from occurring. Preventive care is optimum in order to provide a better and healthier future for all children. RDH
Martha Macaluso, MLT, RDH, BS, is a registered dental hygienist specializing in Orofacial Myofunctional Disorders. She is adjunct faculty at New York University College of Dentistry, where she teaches dental hygiene clinic. Martha is extremely involved in the profession, acting as editor to the Long Island Dental Hygiene Association, delegate to the Dental Hygienist Association of the State of New York, and delegate to the American Dental Hygienists' Association. She is an active member of the International Affiliation of Tongue Tie Professionals, the American Academy of Physiological Medicine and Dentistry, and The Academy of Applied Myofunctional Sciences. She is on the faculty for the Academy of Orofacial Myofunctional Therapy.
Dana Hockenbury, CCC-SLP, COM, is a retired speech pathologist for the New York City Department of Education, and a certified orofacial myologist. She has a full time private practice in Manhattan dedicated to the treatment of orfacial myofunctional disorders. She is an active member, educational chair, and mentor of the International Association of Orofacial Myology (IAOM), as well as a member of the American Academy of Physiological Medicine and Dentistry and the Academy of Applied Myofunctional Sciences (AAMS).
References
1. Hall DM, Renfrew MJ. Tongue tie: Common problem or old wives' tale? Archives of Disease in Childhood 2005. 90:12-11-1215.
2. Wallace H, Clarke S. Tongue tie division in infants with breast feeding difficulties, International Journal of Pediatric Otorhinolaryngology, 2006. Volume 70 issue 7 pages 1257-1261.
3. Kotlow LA. The influence of the maxillary frenum on the development and pattern of dental caries on anterior teeth in breastfeeding infants: prevention, diagnosis, and treatment. Journal of Human Lactation 2010. 26: 304.
4. Kotlow LA. Infant reflux and aerophagia associated with the maxillary lip-tie and ankyloglossia (tongue-tie) Clinical Lactation 2011. Vol. 2-4, 25-29.
5. Kotlow LA. Diagnosing and understanding the maxillary lip-tie (superior labial, the maxillary labial frenum) as it relates to breastfeeding. Journal of Human Lactation. Published online 2 July 2013, DOI: 10.1177/0890334413491325.
6. Kotlow LA. Diagnosis and treatment of ankyloglossia and maxillary frenum in infants using Er: YAG and 1046 diode lasers, European Archives of Paediatric Dentistry.
7. Kotlow LA. Lasers and Soft Tissue Treatments for the Pediatric Dental Patient, Elsevier 2008. Martinelli RL. 2013. Lingual Frenum Protocol with Scores for Infants, CEFAC.
8. Northcutt ME. Overview: the lingual frenum. JCO. Volume XLIII Number 9, 557-565. Fernando C. Tongue Tie - From Confusion to Clarity; A Guide to the Diagnosis and Treatment of Ankyloglossia. Tandem Publications, ISBN: 0646352547.
9. Capsi Pires S, Justo Giugliani ER, Caramez da Silva F. Influence of the duration of breastfeeding on quality of muscle function during mastication in preschoolers: a cohort study. BMC Public Health, 2012. 12:934.
10. Park S. 2009. Sleep Interrupted. Jodev Press.
11. Coryllos E, Watson Genna C, Sallourn A. Congenital tongue-tie and its impact on breastfeeding American Academy of Pediatrics 2004 1-6.
12. Babu H. Surgical Management of Ankyloglossia - A Care Report International Journal of Contemporary Dentistry, November 2010. 1(2).
13. Hazelbaker A. Tongue Tie: Morphogenesis, Impact, Assessment and Treatment, Aiden and Eva Press Books, 2010.
14. Paskay L. OMD Orofacial Myofunctional Disorders: Assessment, prevention and treatment. JAOS. 2012 March-April; 34-40.